Minimally Invasive Tubular Retractor
Minimally Invasive Tubular Retractor utilizing METRx system
Decompression
In preparation for a spinal stenosis procedure, insert the appropriate-sized METRx® System Tube as previously described. Once the Tube is positioned, it is important to extend the laminotomy cephalad above the insertion of the ligamentum flavum.
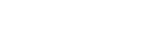
This is to ensure resection of all hypertrophied ligamentum. After the cephalad border of the ligamentum is exposed, it can be separated from the dura using Angled Curettes or a right or left Ball Tip Dissector (Figure 1). The ligamentum is then resected with a 90° or 40° Kerrison Punch (Figure 2). To ensure complete decompression of the lateral recess, the lateral exposure should allow palpation of the inferior pedicle.
This often requires resection of the superior border of the lower lamina (Figure 3). It will also remove any caudal residual ligamentum, which often can compress the dura or nerve root. Foraminotomies are then performed, as necessary, to decompress both exposed foramina (Figure 4). The Ball Tip Probe should be able to pass freely into both the cephalad and caudal foramina.
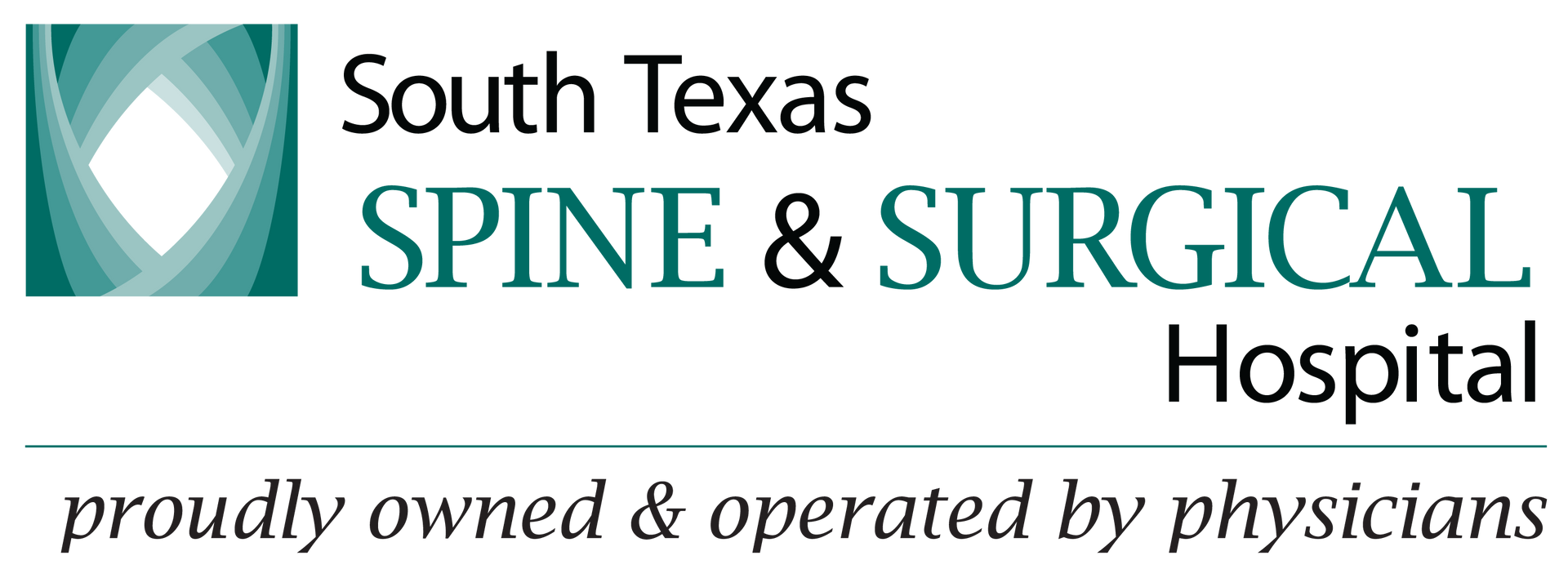
After achieving the ipsilateral decompression, a separate contralateral exposure may be utilized to decompress the opposite lateral recess by following the aforesaid procedural steps (Figure 5).
Contralateral Decompression from an Ipsilateral Approach
As an alternative to contralateral decompression from the contralateral side, an ipsilateral approach to contralateral decompression can be utilized. After completion of the ipsilateral decompression, the Tubular Retractor is angled medially to expose the anterior spinous process. An osteotome or a high speed drill can then be used to resect the anterior spinous process and the medial aspect of the contralateral lamina (Figure 6).
This exposes the contralateral hypertrophied ligamentum flavum, which can then be resected using Kerrison Punches and Curettes (Figures 7a, 7b, and 7c). Care is taken to palpate the caudal pedicle and probe both the cephalad and caudal foramina to be certain that the decompression is complete (Figure 8).
Discectomy utilizing the METRx® System
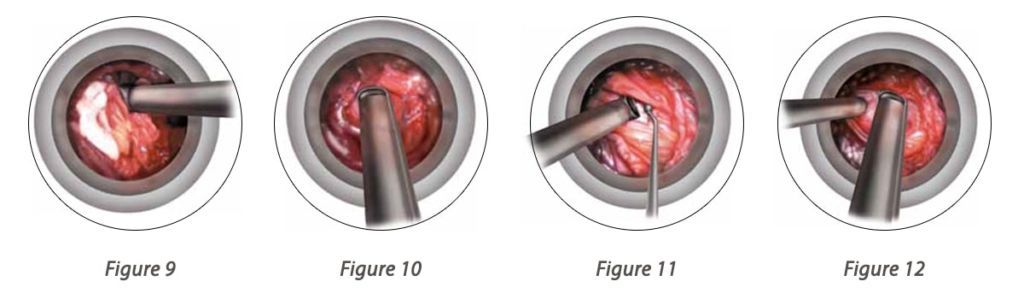
Soft Tissue Removal and Laminar Identification
It is essential to remove all soft tissue exposed in the operative corridor in order to maximize the working space within the Tubular Retractor. This can be accomplished with a Pituitary Rongeur and/or electrocautery. The laminar edge is identified and the ligamentum flavum is detached from the undersurface of the lamina with a small Angled Curette (Figure 9).
Laminar and Interlaminar Space Identification
A hemilaminotomy/medial facetectomy is then performed with a Kerrison Punch or high speed drill (Figure 10). Lateral recess and/or foraminal stenosis can be addressed in this fashion. Effective utilization of lateral fluoroscopy will help tailor the dissection as necessary to access specific pathology. When the decompression is done mainly for lumbar stenosis and not a disc herniation, the laminotomy is carried just cephalad to the insertion of the ligamentum flavum onto the underside of the lamina. This assures that all hypertrophied ligamentum will be removed, adequately decompressing the canal. If the pathology is beyond the confines of the Tubular Retractor, wanding can be used to reposition the Tubular Retractor.
Ligamentum Flavum Removal
The ligament is penetrated with the Curette or Ball Probe utilizing a twisting motion under the remaining superior lamina where the ligament is thin (Figure 11). It is peeled back caudally and dorsally, then resected with a Kerrison Punch (Figure 12).
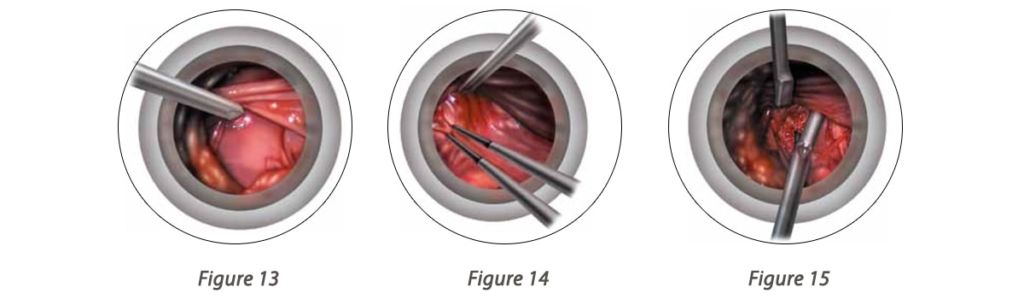
Nerve Root Exploration and Retraction
There is an initial tendency to “cone” the exposure down to the final target reducing the working space and visualization in the Tubular Retractor. In order to avoid this, it is important to complete soft tissue, bone, and ligament removal over the entire area of the exposure. Figure 13 shows appropriate exposure of the epidural space
The dura and traversing nerve root are identified. The nerve root is retracted medially utilizing a Penfield Dissector, Love style, or Suction Retractor (Figure 13). The volar epidural space can then be explored. If necessary, epidural veins can be cauterized with bipolar forceps and divided with micro scissors (Figure 14). Cotton patties can also be used to obtain hemostasis.
Discectomy and Closure
Identify the disc herniation. If an annulotomy is necessary, it can be accomplished with the Micro Scissors while protecting the nerve root with the Retractor. The herniated disc is then removed with a Pituitary Rongeur in a standard fashion (Figure 15). Intradiscal and extradiscal work can be carried out as one would normally perform during an open microdiscectomy. The nerve root is explored to ensure the decompression is complete.
Once the nerve root is decompressed, irrigate the disc space thoroughly. Epidural steroids may be injected if desired. Loosen the Flexible Arm assembly and slowly remove the Tubular Retractor. Any bleeding in the paraspinal musculature can be controlled with the bipolar forceps as the Tube is removed.
The METRx® System allows access to the spine using a series of sequential muscle dilation tubes.
This dilation approach causes less disruption to the surrounding muscles and also allows the paraspinous muscles to remain attached to the spinous process. The minimally invasive implants and instruments require smaller incisions than traditional open surgery and are designed for muscle-sparing approaches.